Clinical Success
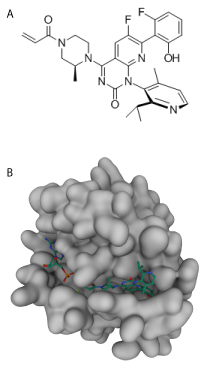
Additional optimization efforts were needed to improve cellular potency for therapeutic viability. Amgen, in collaboration with Carmot therapeutics, was developing a Cys-12 covalent small molecule, and their initial compound showed multi-fold enhancement in potency compared to ARS-1620 in part through binding a cryptic pocket comprised of Y96/H95/Q99 in KRASG12C (6). Unfortunately, the biopharmaceutical properties of this drug were unsuitable. The group went through many rounds of modifications to identify a drug that could capitalize on interacting with the cryptic pocket to maintain potency while enhancing its bioavailability, which also required overcoming a configurational stability issue. The result was the identification of AMG510 (Sotorasib), which was the first Cys-12 covalent KRASG12C inhibitor tested in clinical trials (7). It showed great promise in phase I clinical trails with demonstrated anti-tumor activity (8). Importantly, of the 129 patients treated with Sotorasib no dose-limiting toxic effects or treatment-related deaths were observed. Of the patients with NSCLC 32.2% had an objective response and 88.1% had disease control. In the Codebreak 1000 phase II clnical trials similar positive results were reported with an objective response rate of 36% and a objective response rate of 81% (reviewed in (9)). These results provided the groundwork for the FDA’s accelerated approval to use Sotorasib as a therapy for NSCLC.
Acquired Resistance and Summary
Sotorasib has been a monumental success by any measure; still, there is evidence in preclinical models that acquired resistance will be problematic(10). Recently, Tanaka et al. sought to identify mechanisms by which acquired resistance occurred to KRASG12C targeting drugs, and they determined that 10 heterogenous alterations occurred in a patient with acquired resistance(11). These alterations targeted four genes, KRAS, NRAS, BRAF, and MAP2k1, all of which converged to reactive the RAS-MAPK signaling. Looking closer at KRAS led to the identification of a KRAS Y96D mutation which altered the switch-II pocket and suppressed drug interaction. This escape mechanism was validated in KRASG12C cancer models. New investigation into next generation drugs will be necessary to overcome this acquired resistance, and Cytoskeleton is proud to offer a panel of RAS tools to aide in these studies.
References
1. Adderley H, Blackhall FH, Lindsay CR. KRAS-mutant non-small cell lung cancer: Converging small molecules and immune checkpoint inhibition. EBioMedicine. 2019;41:711-6.
2. Ghimessy A, Radeczky P, Laszlo V, Hegedus B, Renyi-Vamos F, Fillinger J, et al. Current therapy of KRAS-mutant lung cancer. Cancer Metastasis Rev. 2020;39(4):1159-77.
3. John J, Sohmen R, Feuerstein J, Linke R, Wittinghofer A, Goody RS. Kinetics of interaction of nucleotides with nucleotide-free H-ras p21. Biochemistry. 1990;29(25):6058-65.
4. Ostrem JM, Peters U, Sos ML, Wells JA, Shokat KM. K-Ras(G12C) inhibitors allosterically control GTP affinity and effector interactions. Nature. 2013;503(7477):548-51.
5. Janes MR, Zhang J, Li LS, Hansen R, Peters U, Guo X, et al. Targeting KRAS Mutant Cancers with a Covalent G12C-Specific Inhibitor. Cell. 2018;172(3):578-89 e17.
6. Lanman BA, Allen JR, Allen JG, Amegadzie AK, Ashton KS, Booker SK, et al. Discovery of a Covalent Inhibitor of KRAS(G12C) (AMG 510) for the Treatment of Solid Tumors. J Med Chem. 2020;63(1):52-65.
7. Canon J, Rex K, Saiki AY, Mohr C, Cooke K, Bagal D, et al. The clinical KRAS(G12C) inhibitor AMG 510 drives anti-tumour immunity. Nature. 2019;575(7781):217-23.
8. Hong DS, Fakih MG, Strickler JH, Desai J, Durm GA, Shapiro GI, et al. KRAS(G12C) Inhibition with Sotorasib in Advanced Solid Tumors. N Engl J Med. 2020;383(13):1207-17.
9. Sotorasib Edges Closer to Approval. Cancer Discov. 2021;11(5):OF2.
10. Koga T, Suda K, Fujino T, Ohara S, Hamada A, Nishino M, et al. KRAS Secondary Mutations That Confer Acquired Resistance to KRAS G12C Inhibitors, Sotorasib and Adagrasib, and Overcoming Strategies: Insights From the In Vitro Experiments. J Thorac Oncol. 2021.
11. Tanaka N, Lin JJ, Li C, Ryan MB, Zhang J, Kiedrowski LA, et al. Clinical acquired resistance to KRASG12C inhibition through a novel KRAS switch-II pocket mutation and polyclonal alterations converging on RAS-MAPK reactivation. Cancer Discov. 2021.